Diabetic Retinopathy
Understanding Diabetic Retinopathy
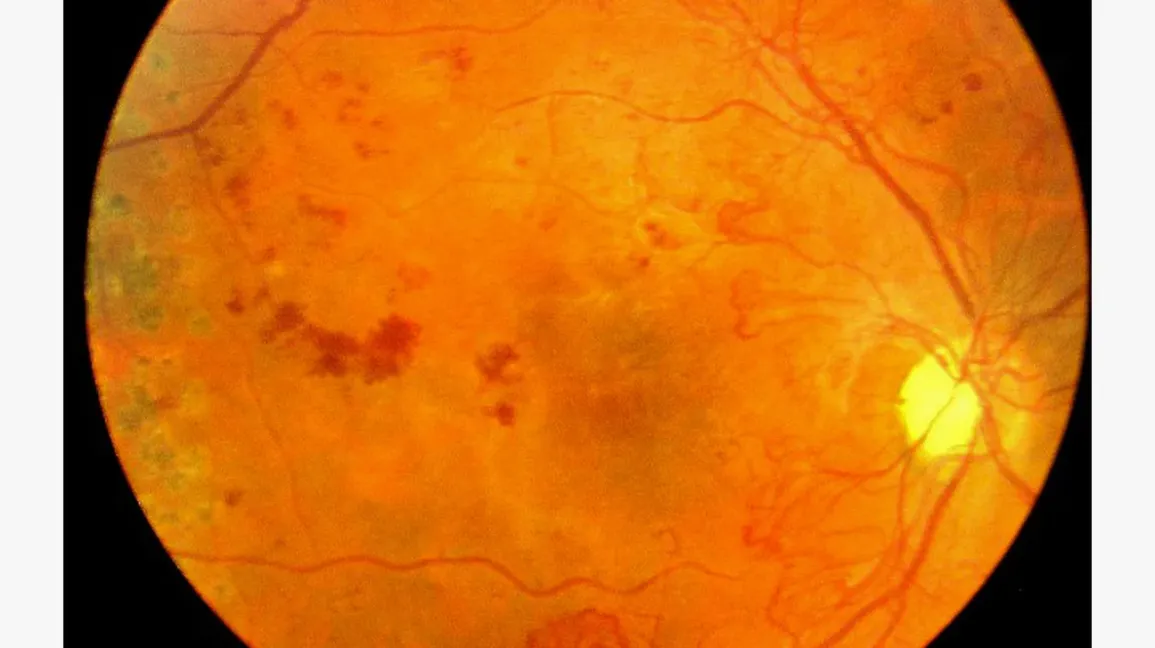
Diabetic retinopathy results from damage to the tiny blood vessels in the retina, which become leaky, blocked, or both. The condition progresses in two stages:
- Non-Proliferative Diabetic Retinopathy (NPDR): Early-stage retinopathy features changes like microaneurysms, small hemorrhages, and “cotton wool spots” (areas of blocked capillaries), which typically don’t impact vision but may progress over time.
- Proliferative Diabetic Retinopathy (PDR): Advanced retinopathy can lead to the growth of abnormal blood vessels on the retina. These vessels may bleed (causing vitreous hemorrhage) and create scar tissue, which can lead to retinal detachment and severe vision loss if left untreated.
Two key forms of vision loss related to diabetic retinopathy are:
- Clinically Significant Macular Edema (CSMO): Excessive leakage from retinal capillaries causes swelling in the macula, leading to vision impairment. This is the most common cause of vision loss in diabetics.
- Proliferative Diabetic Retinopathy (PDR): Blocked retinal capillaries lead to ischemia, stimulating abnormal blood vessel growth on the retina’s surface, which can result in serious complications, including retinal detachment and severe vision loss.
Managing Diabetic Eye Disease
Managing diabetic retinopathy requires a comprehensive approach, including regular examinations and imaging tests like fundus photography, OCT (Optical Coherence Tomography), and fluorescein angiography. These tools enable detailed assessment of the retina, helping guide treatment strategies. Coordination between your ophthalmologist, family doctor, and diabetes specialist is essential, as factors like blood sugar control, blood pressure, and kidney health influence the severity of retinopathy.
Treatment Options for Diabetic Retinopathy
Effective treatment for diabetic retinopathy is multi-faceted, aiming to preserve vision and prevent further damage:
- Optimize Systemic Health: Controlling blood sugar and blood pressure can slow retinopathy development by up to 75% and reduce progression by 50%.
- Retinal Laser Therapy: Laser treatment is the cornerstone of retinopathy care, especially for proliferative cases, reducing abnormal blood vessel growth by creating small scars in the peripheral retina. This treatment typically requires multiple sessions.
- Supplementary Treatments: For severe cases, intraocular injections and micro-incisional vitrectomy surgery may be used alongside laser.
Specific Treatments for CSMO and PDR
- CSMO Treatment: Treatment begins with gentle laser therapy to the swollen areas of the macula, though more advanced cases may require medication injections like Avastin, Lucentis, or Triamcinolone to reduce swelling and improve vision.
- PDR Treatment: Immediate laser treatment is needed to prevent the growth of abnormal blood vessels, supplemented by injections and surgery when necessary. While PDR laser therapy can be extensive and may cause temporary vision changes, timely treatment is critical to prevent blindness.
In cases of severe complications, such as vitreous hemorrhage or retinal detachment, vitrectomy surgery may be required to prevent further vision loss.
Through diligent monitoring and timely intervention, the progression of diabetic retinopathy can be controlled, preserving vision and enhancing quality of life for individuals with diabetes.